Shane Reichart's Posts (1)
Deliverance At Delivery
May 8, 2025 - Shane Reichart
A Roller Coaster Pregnancy
With praise to the Lord, our first child, Vienna Ruth Reichart, was born at 4:31am on April 30th, 2025! She was 7 lbs., 12 oz., and 20.9 in. long. Despite some harrowing events along the journey, Mommy and "Little V" are now home and recovering well.
What follows is a lengthy read with details I'm recording for our own posterity and for Vienna's diehard fanbase.

Namesake
Although every father wants a daughter named after cured meat, Vienna is named after the city, not the sausage. While Amanda and I traveled around Europe for three months in 2023, we noted that people often name their children after cities, and strangely, not countries. We talked about countries that would make good names, such as "Iceland" for a boy and "Belize" for a girl. "Czechoslovakia" was never on the table.
But then, as we prepared to travel to Austria's capital, we agreed it was a pretty name and were surprised it wasn't a popular girl's name, as are "Paris," "Charlotte," "Sydney," and "Oklahoma City." While strolling the beautiful streets and gardens of Vienna, Amanda daydreamed about having a little girl named "Vienna" someday. And now she does! I had daydreamed that day about having an "Amanda, Jr.," but Amanda, Sr. promptly vetoed the idea. Several nurses mentioned her name sounds "regal." We agree.

The First Big Drop
The first drop on our pregnancy roller coaster was a big one, late in the first trimester on a Saturday evening. Amanda thought we'd lost our baby when she had substantial bleeding one morning. I tried to reassure my heartbroken wife that we didn't know anything with certainty yet and that it could be a different complication. Fortunately, Amanda already had a checkup appointment scheduled for the following Monday morning when the offices reopened, so her perceived eternity of waiting for answers was actually only about thirty-six hours. (Thirty-six hours would become a recurring timeframe.)
The answer came in the form of a cervical polyp, which had burst. Thank the Lord, our developing little baby was unaffected, but frequent bleeding throughout the pregnancy, although still alarming each time, would be our new normal. (Surgery to remove the polyp would be too risky to perform while Amanda was pregnant.)
A Looming Drop That Never Happened
A few months later, an ultrasound revealed a uterine hematoma. If it were to burst, the internal bleeding in the womb would put Vienna at tremendous risk, so Amanda was put on a lifting restriction by her doctor and was therefore unable to work until it healed. This was a blessing in disguise because, since she was on medical disability, we had an unexpected opportunity to visit my family in Illinois for Thanksgiving. (We had already planned to use her remaining vacation time to visit her family for Christmas.) About a month later, the hematoma could no longer be found, so Amanda was able to return to work just after Thanksgiving.

Just a Bumpy Ride
The next few months of pregnancy were fairly uneventful, except for the little bumps of recurring bleeding. While the pregnancy was progressing along without additional complications, we had, in the meantime, purchased our new home, which I began remodeling so we could move in before our apartment lease expired a couple months later. To be clear, life in general was absolutely not uneventful!
That first drop in the roller coaster of pregnancy would become child's play when compared to the fully inverted loop we were about to endure. We tell everyone who asks that Amanda's labor was thirty-six hours. It might have been longer. Here's the scoop on the big vertical loop.
Labor Begins?
Amanda's "water" ("waters" in British English) broke early in the morning of Saturday, April 26th, but it was just a trickle. She called the hospital to inquire about it because there are a few other pregnancy-related things it could have been. (You probably already thought of one of them.) The nurse on the phone determined it likely was not her water breaking. However, by Monday, April 28th, Amanda was becoming pretty certain the virtual assessment was incorrect. Fortunately, she had already scheduled a checkup later that afternoon, during which they determined she was already 1 cm dilated and 90% effaced and that her water had broken after all—probably since Saturday morning—so we needed to get to the hospital promptly.

No Room in the Inn
Apparently, everyone else, including my best friend Matthew Rennels and his wife, was trying to coordinate their child's birthdate with ours, so when we arrived at the hospital that evening, there was no room in the inn. Instead, after a little wait, we were admitted into a room within the emergency department. (Certainly, better accommodations than a stable!) Four hours later, about the time we felt settled in, we were able to move from the emergency room to our second room in the labor and delivery department.
Emily, a dear sister in Christ and co-leader of the church small group of which we were part (before we started our own), met us in this room to act as an informal doula. We're so grateful, and she did a stellar job. 5 stars.
Who You Callin' "Practice Contractions"?
To further complicate the timeline of when Amanda's labor began, her so-called practice contractions (a.k.a. "Braxton-Hicks") began to be notably long and strong a few weeks before her water broke. On a couple of occasions, she was completely incapacitated by them; she thought she was going into labor. These early contractions ended up being more painful than the contractions that began after labor was induced, so we're unclear when practice contractions became real contractions. Therefore, we consider the "start" of labor as the moment when we checked into the hospital, a full sixty hours after her water broke.
Expectin' an Infection
Shortly after we arrived at the hospital, Amanda was given medicine to induce/expedite labor. This was because of the high risk of uterine infection since her water had been ruptured for so long. Eventually, that risk of infection became a reality as Amanda's temperature continued to climb, so she was given antibiotics intravenously to protect the baby from fever temperatures and from an infection of her own.

Amanda is Superhuman
Thirty-two hours after we arrived at the hospital, just after midnight on Wednesday, April 30th, Amanda was dilated to 10 cm and the doctor had her begin pushing, which took over four grueling hours. Amanda was superhuman. The nurses were amazed at her stamina, determining she must be an athlete. The reality was that she had no idea it had been that long, and she was just eager to see her baby! She's also superhuman if I didn't mention it already.
Between contractions, she was her usually chatty self, talking about, among other things, how the doctor and nurses needed to watch comedian Nate Bargatze as George Washington on SNL. (You should, too.) She had often prayed that she would be kind to me during labor, and God granted that request. Her kindness overflowed to everyone in the room! Thank God and thank Michael J. Epidural.
After about three and a half hours, the doctor noticed Vienna's heart rate falling. She said it was likely because our baby girl was understandably exhausted from the prolonged delivery, but the doctor called for the NICU team to be available in the delivery room as a precaution in case it was related to the infected amniotic fluid in which Vienna was still suspended.
A Tear Down There
When Vienna's head finally emerged, the rest of her followed in what seemed like a burst with excessive blood. If I understood what was happening correctly, the placenta came out as a single birth with Vienna. At least some of the excessive bleeding was because Amanda had a stage 3C tear (out of 4). If you are at all squeamish, I recommend against investigating this scale, so suffice it to say we're not talking about a small tear. I heard the doctor state that Amanda was hemorrhaging, but it was unclear if that was in reference to the tear or to a separate complication. (I'll speculate on this later.)

Free-Falling off the Track
As traumatic as Amanda's side of the delivery was, all of our concern was immediately directed to Vienna instead. Her umbilical cord was wrapped around her body twice—once tightly around her neck and a second time also around her upper chest, constricting both her breathing and the oxygenated blood flow through the umbilical cord. Any parent's greatest fear was realized in that moment. Our baby girl was deeply blue and completely lifeless. Our roller coaster just went entirely off the track.
The doctor placed her on her Mommy's belly for half a moment to slice the tangled umbilical cord from around Vienna's body. Then, a nurse immediately rushed her across the room to the awaiting NICU team. (So, no, I was given no opportunity to cut the cord.) While the doctor proceeded to quickly stitch Amanda back up to stop her hemorrhaging, the NICU team was abuzz saving Vienna's precious little life.
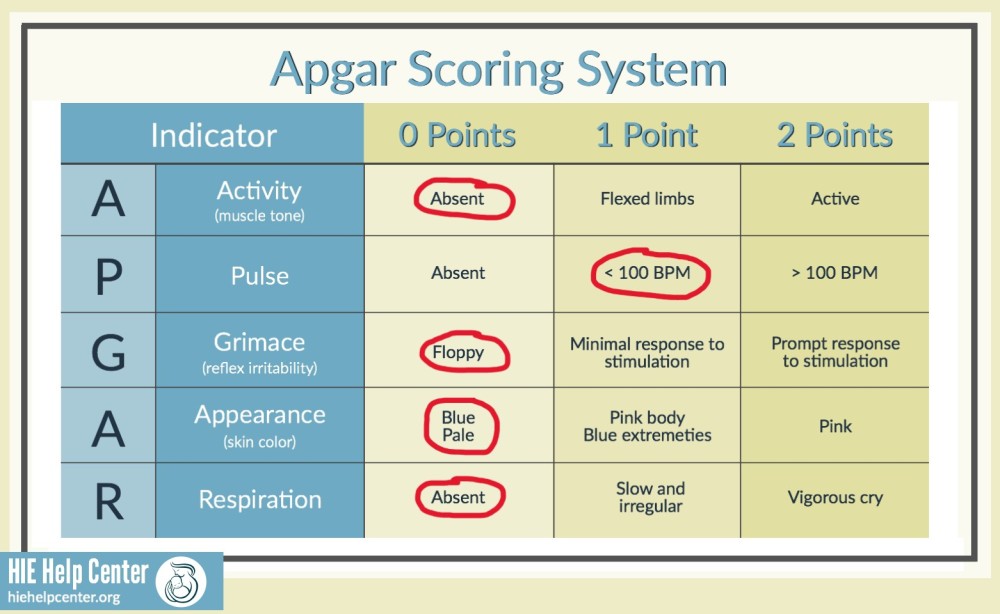
The APGAR score is used to assess a baby's health at birth. A perfect score is 10. Little V had a score of 1. She wasn't breathing, was completely limp and non-responsive, and was as blue as the keyboard cover with which I'm typing this post. The only reason she didn't score a 0 is because she had a weak but detectable pulse.
The team immediately placed an oxygen mask over her face and began working her chest to get her breathing. She began breathing for a moment, so they removed the oxygen mask to feed a vacuum tube down her throat to remove excess (and likely infected) amniotic fluid from her lungs. That was productive, but she quit breathing again, so they had to resort to supplying oxygen again. I was as close as they would let me be, praying over her tiny, lifeless body.
Amanda was still across the room on the gurney with Emily tending to her, so she was looking to me for reassurance that everything was okay, which it absolutely was not. Our baby was barely alive. But I trusted the Lord that everything would be okay. And the NICU team at work had a general tone of urgency, but not emergency. I mouthed across the room to Amanda that everything would be okay, which is what I think any other husband would do in this situation. (Mentally note this moral dilemma for your next debate about the black-and-white ethics of lying.) I also gave her two thumbs up, which is what I think any other dad would do in this situation. But my furrowed face communicated that this optimistic assessment was tempered with genuine concern.
By the five-minute benchmark, Vienna scored a 5, which is still a failing score warranting further intervention. Her skin color graduated to "pale," and she began moving her arms slightly when prodded. With a little more oxygen and a lot of prayer, she began to perk up and even soiled her diaper. She whimpered but never cried, and at 10 minutes she scored an 8. A score of 7 is considered "passing," so they were finally able to take her to her mother's chest for skin-to-skin contact, which helps a baby regulate temperature and breathing—help she much needed!

By now our baby had turned red, so we had two out of three primary colors covered. It took about a half-hour for Vienna to properly fuss, and she ceased as quickly as she started. I think she was as reluctant as we were to complain about anything because she was so grateful to be alive!
If you know the Lord, can you take a moment to praise him with me now?
Also, in retrospect, I wonder if the reason Amanda did not have to push again to deliver the afterbirth was because the usual slack in the umbilical cord was taken up by being wrapped around Vienna's body twice. If so, as Amanda pushed the baby, the tightly tethered placenta was simultaneously being torn from the uterine wall. Again, I'm speculating here, but if this was the case, it certainly explains the lack of oxygen in Vienna's body and the excessive bleeding in Amanda's.
We didn't find out about Vienna's APGAR scores until we were moved into our third room for postpartum recovery and I inquired about them from a nurse. She was surprised to see the score of 1 on Vienna's chart because what she had observed was a healthy and happy baby! After a couple of mildly concerning dips in body temperature during Vienna's first day of life, all her vitals were looking good! Amanda and I are glad we didn't know her APGAR score during delivery because in those early moments, we were permitted to wonder if the complications we witnessed were more common than they seemed.

Back on Track
Our roller coaster appeared to be on a straight track back to the corral for passenger unloading.
However, thirty-six hours later, during Vienna's second day of life, we began being concerned because she had only wet a few diapers, without a dirty diaper since the early one in the delivery room. Also, she seemed to be spitting up everything she took in. The nurses encouraged us not to worry because it was likely amniotic fluid she was spitting up, and it had to work through her system. I wasn't convinced because her spit-up was bright yellow—much more so than her mother's milk.
On her third day, I was pushing Vienna around the hallways in her rolling bassinet so Amanda could get some much-needed rest... Oh, by the way, don't take a newborn baby for a walk outside of the postpartum wing, or it will trigger a lockdown of the hospital. (I narrowly avoided this DEFCON level by mentioning to a nurse, in passing, that I was headed to another part of the building to get my wife the "good" coffee.) ... So again, while Amanda was sleeping and I was taking Vienna for this "walk," she spit up twice, so I wheeled her to a nurse and insisted it was brighter yellow than Amanda's colostrum and it likely contained bile. She humored me and had her supervisor take a look.

The supervisor took it much more seriously, quickly informing me they'd like to admit her into the nursery to run tests. The nursery bore the name of the very woman with whom I was speaking, so I knew Vienna would be in good hands in what was now her fourth room! When Mommy woke up, she was sure surprised to see Daddy empty-handed!
Bonus Thrill
Those tests confirmed my suspicion that bile was present in Vienna's spit-up and that my concern was legitimate. Also, while in the nursery, they discovered crystallized urea in her diaper where liquid urine should be. Vienna was unable to keep any milk down, so she was getting severely dehydrated. On Vienna's third day, Friday, May 2nd, after a few hours of scans and tests that revealed no obvious causes, the team was still unable to keep fluids in Vienna's little body. They decided to simultaneously discharge Amanda from postpartum recovery and admit "Little V" into the NICU. It turns out our roller coaster had a hidden track that nosedived for one last thrill.
The NICU was Vienna's fifth and final room in the hospital. She was intubated through her nose so they could administer fluids into her stomach at a pace that she could actually, um, stomach, without spitting up. A successful urination would be a sign of improvement, so we began praying for pee. (Is that book title taken?) She did have one wet diaper the next day, but it was bright orange. Among other possibilities, this is an early indicator of kidney failure from dehydration.

The NICU nurses said that if she didn't begin wetting her diapers consistently soon, they would need to administer fluids intravenously. Vienna must have heard the plan because within an hour, she mustered all the urine she could to fully wet her diaper with the typical yellow we were all hoping to see. She was also just beginning to nurse again after being fed only by tube for a couple of days!
However, we weren't out of the woods yet. (I think I just switched my coaster metaphor from roller to alpine.) Vienna still hadn't produced a soiled diaper, and that was a lingering concern of a possible larger digestive issue that caused the dehydration in the first place. But the fact that she was now retaining fluids gave us hope that her digestive system had received the jump start it needed to get moving. Our little chameleon also successfully completed the palette of primary colors by turning yellow from jaundice, so they began monitoring that as well.

She otherwise seemed healthy and happy. She was the largest baby in the NICU because the other baby residents were born prematurely. She managed to pull her nasal feeding tube out at least once, and even our wonderful and experienced nursing staff failed to keep her little hands swaddled. She may have her mother's face and grace, but she has her father's ingenuity! I couldn't even count the number of times she pulled the electrodes off her little chest and belly.
Split Track
Meanwhile, Amanda's postpartum recovery was progressing well. She still had limited mobility, which was to be expected with the degree of tearing she endured. So, I was serving as her personal assistant for most activities that didn't involve the restroom or breasts. (I'd have done these activities for her, too, if I could!)

Is there a roller coaster in which the individual cars separate and go on different tracks? (Disney's Haunted Mansion, maybe?) In our NICU room, there was a small couch that could serve as a single (smaller than twin) bed in a pinch—useful, perhaps, for napping, but not ideal for overnight stays. Since Amanda needed quality rest for her own recovery and still counted on my assistance for many tasks, we made the difficult decision to sleep at home instead of the NICU so we could be together.
Food was not allowed in the NICU rooms, so I had been escorting Amanda on my arm as she shuffled down the hall to the NICU parents' lounge for meals. Staying at home overnight also meant adding a long shuffle to and from the car each night and morning. Both of my ladies were struggling!
Finally, at the end of Vienna's fourth day, as we were preparing to leave for the night to sleep at home, she soiled her diaper for the first time since the early one a few minutes after birth. Praise the Lord for poop! We slept better that night than any other since labor began. I almost wrote that we "slept well," but who am I kidding? We were awake for nearly an hour out of every three throughout the night trying to figure out breast-pumping at home, without the assistance of a nurse. We also rushed back to the NICU each morning to see and feed our daughter so she could get as much of her mother's milk as possible instead of supplemental nutrition.

On Track to the Corral
When we returned the following morning, "Little V" had apparently soiled ALL the diapers! We were relieved that her bowels were working and, honestly, that we had a team of nurses changing her diapers that night. Her appetite returned, and she was able to drink enough milk through her mouth that they began weaning her off the tube. We knew it was just a matter of time before they would let Vienna go home. And as long as I didn't get trapped in our private bathroom again, I'd be able to go home with her. Oh, didn't I mention I got trapped in the bathroom? I did. The door jammed. Amanda had to call the staff to get me out.
Even though we were in the NICU doesn't mean it was all somber and sad. We had wonderful moments together! One evening, I pulled down the window blinds and pointed at them a portable movie projector so we could have our first movie night together. We watched The Lion King. The nurses thought it was epic. They were right.

Home, Sweet Home
Finally, on Wednesday, May 7th, a week after she was born, we were able to take Vienna home. Praise the Lord. Now, she truly is healthy, happy, and energetic. You would never know, and she certainly doesn't, that she had such a rough start. She fusses only when her diaper needs to be changed or when she is hungry. Given her history, these are both very welcome fusses.
We were overly impressed with our experience at Cone Health's Women & Children's Center. The staff were kind, friendly, available, and knowledgeable. If you plan to have a complicated and highly emotional delivery like ours, I couldn't recommend a better place to have it.
Meal Train
We could use your help with meals! Please consider picking a slot on our Meal Train schedule to provide us with a meal we don't have to make ourselves.